Key Points
-
Mature B-cell malignancies are initiated often by errors in immunoglobulin gene variable–diversity–joining region (VDJ) recombination, somatic hypermutation and/or class-switch recombination that lead to chromosomal translocations. Dysregulation of the genes at the translocation breakpoints disrupts B-cell homeostasis by perturbing proliferation, apoptosis and differentiation.
-
Advances in molecular analyses, in particular gene-expression profiling, have increased the precision of diagnosis for lymphoid malignancies. These methods have shown that lymphomas and leukaemias can share gene-expression programmes with their normal cellular counterparts. Molecular profiling has shown that some of the diagnostic categories that are used at present consist of many molecularly distinct diseases that cannot be distinguished morphologically.
-
Antigenic stimulation and selection have crucial roles in the pathogenesis and persistence of some lymphomas and leukaemias. The identification and elimination of an antigenic stimulus can eradicate some tumours.
-
Improved molecular classification and an understanding of the pathogenetic mechanisms that are involved in lymphoid malignancies are providing new molecular targets for therapy.
Abstract
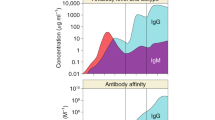
When the regulation of B-cell differentiation and activation is disrupted, lymphomas and leukaemias can occur. The processes that normally create immunoglobulin diversity might be misdirected, resulting in oncogenic chromosomal translocations that block differentiation, prevent apoptosis and/or promote proliferation. Prolonged or unregulated antigenic stimulation might contribute further to the development and progression of some malignancies. Lymphoid malignancies often resemble normal stages of B-cell differentiation, as shown by molecular techniques such as gene-expression profiling. The similarities and differences between malignant and normal B cells indicate strategies for the treatment of these cancers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Fugmann, S. D., Lee, A. I., Shockett, P. E., Villey, I. J. & Schatz, D. G. The RAG proteins and V(D)J recombination: complexes, ends and transposition. Annu. Rev. Immunol. 18, 495–527 (2000).
Marculescu, R., Le, T., Simon, P., Jaeger, U. & Nadel, B. V(D)J-mediated translocations in lymphoid neoplasms: a functional assessment of genomic instability by cryptic sites. J. Exp. Med. 195, 85–98 (2002).
Boehm, T. et al. Alternating purine–pyrimidine tracts may promote chromosomal translocations seen in a variety of human lymphoid tumours. EMBO J. 8, 2621–2631 (1989).
Welzel, N. et al. Templated nucleotide addition and immunoglobulin JH-gene utilization in t(11;14) junctions: implications for the mechanism of translocation and the origin of mantle-cell lymphoma. Cancer Res. 61, 1629–1636 (2001).
Yu, W. et al. Continued RAG expression in late stages of B-cell development and no apparent re-induction after immunization. Nature 400, 682–687 (1999).
Gartner, F., Alt, F. W., Monroe, R. J. & Seidl, K. J. Antigen-independent appearance of recombination activating gene (RAG)-positive bone-marrow B cells in the spleens of immunized mice. J. Exp. Med. 192, 1745–1754 (2000).
MacLennan, I. C. Germinal centers. Annu. Rev. Immunol. 12, 117–139 (1994).
Liu, Y. J., Zhang, J., Lane, P. J., Chan, E. Y. & MacLennan, I. C. Sites of specific B-cell activation in primary and secondary responses to T-cell-dependent and T-cell-independent antigens. Eur. J. Immunol. 21, 2951–2962 (1991).
Chua, K. F., Alt, F. W. & Manis, J. P. The function of AID in somatic mutation and class-switch recombination: upstream or downstream of DNA breaks. J. Exp. Med. 195, F37–F41 (2002).
Honjo, T., Kinoshita, K. & Muramatsu, M. Molecular mechanism of class-switch recombination: linkage with somatic hypermutation. Annu. Rev. Immunol. 20, 165–196 (2002).
Papavasiliou, F. N. & Schatz, D. G. Somatic hypermutation of immunoglobulin genes: merging mechanisms for genetic diversity. Cell 109, S35–S44 (2002).
Pelicci, P. G., Knowles, D. M. 2nd, Magrath, I. & Dalla-Favera, R. Chromosomal breakpoints and structural alterations of the c-myc locus differ in endemic and sporadic forms of Burkitt lymphoma. Proc. Natl Acad. Sci. USA 83, 2984–2988 (1986).
Rabbitts, T. H., Hamlyn, P. H. & Baer, R. Altered nucleotide sequences of a translocated c-myc gene in Burkitt lymphoma. Nature 306, 760–765 (1983).
Goossens, T., Klein, U. & Kuppers, R. Frequent occurrence of deletions and duplications during somatic hypermutation: implications for oncogene translocations and heavy-chain disease. Proc. Natl Acad. Sci. USA 95, 2463–2468 (1998).
Pasqualucci, L. et al. BCL-6 mutations in normal germinal-center B cells: evidence of somatic hypermutation acting outside Ig loci. Proc. Natl Acad. Sci. USA 95, 11816–11821 (1998).
Shen, H. M., Peters, A., Baron, B., Zhu, X. & Storb, U. Mutation of BCL-6 gene in normal B cells by the process of somatic hypermutation of Ig genes. Science 280, 1750–1752 (1998).
Pasqualucci, L. et al. Hypermutation of multiple proto-oncogenes in B-cell diffuse large-cell lymphomas. Nature 412, 341–346 (2001). This study shows that diffuse large B-cell lymphomas (DLBCLs) can accumulate mutations in non-immunoglobulin genes as a result of somatic hypermutation (SHM).
Neri, A., Barriga, F., Knowles, D. M., Magrath, I. T. & Dalla-Favera, R. Different regions of the immunoglobulin heavy-chain locus are involved in chromosomal translocations in distinct pathogenetic forms of Burkitt lymphoma. Proc. Natl Acad. Sci. USA 85, 2748–2752 (1988).
Bergsagel, P. L. et al. Promiscuous translocations into immunoglobulin heavy-chain switch regions in multiple myeloma. Proc. Natl Acad. Sci. USA 93, 13931–13936 (1996).
Jacob, J., Kelsoe, G., Rajewsky, K. & Weiss, U. Intraclonal generation of antibody mutants in germinal centers. Nature 354, 389–392 (1991).
Han, S. et al. Cellular interaction in germinal centers. Roles of CD40 ligand and B7-2 in established germinal centers. J. Immunol. 155, 556–567 (1995).
Kawabe, T. et al. The immune responses in CD40-deficient mice: impaired immunoglobulin class switching and germinal center formation. Immunity 1, 167–178 (1994).
Weller, S. et al. CD40–CD40L-independent Ig gene hypermutation suggests a second B-cell diversification pathway in humans. Proc. Natl Acad. Sci. USA 98, 1166–1170 (2001).
Matsumoto, M. et al. Affinity maturation without germinal centres in lymphotoxin-α-deficient mice. Nature 382, 462–466 (1996).
William, J., Euler, C., Christensen, S. & Shlomchik, M. J. Evolution of autoantibody responses via somatic hypermutation outside of germinal centers. Science 297, 2066–2070 (2002). References 23–25 provide evidence for SHM in the absence of recognizable germinal centres (GCs).
Alizadeh, A. A. et al. Distinct types of diffuse large B-cell lymphoma identified by gene-expression profiling. Nature 403, 503–511 (2000).
Shaffer, A. L. et al. Signatures of the immune response. Immunity 15, 375–385 (2001).
Alizadeh, A. et al. The Lymphochip: a specialized cDNA microarray for the genomic-scale analysis of gene expression in normal and malignant lymphocytes. Cold Spring Harb. Symp. Quant. Biol. 64, 71–78 (1999).
Rosenwald, A. et al. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N. Engl. J. Med. 346, 1937–1947 (2002). References 26 and 29 show the utility of gene-expression profiling for the analysis of human B-cell lymphomas, and show that a single diagnostic category (DLBCL) is composed of many molecularly distinct diseases with different clinical outcomes.
Lossos, I. S. et al. Ongoing immunoglobulin somatic mutation in germinal center B-cell-like, but not in activated B-cell-like, diffuse large-cell lymphomas. Proc. Natl Acad. Sci. USA 97, 10209–10213 (2000).
Davis, R. E., Brown, K. D., Siebenlist, U. & Staudt, L. M. Constitutive nuclear factor-κB activity is required for survival of activated B-cell-like diffuse large B-cell lymphoma cells. J. Exp. Med. 194, 1861–1874 (2001). This work shows that the NF-κB pathway is constitutively active in activated B-cell-like DLBCLs, and that it is a potential therapeutic target.
Angelin-Duclos, C., Cattoretti, G., Lin, K. I. & Calame, K. Commitment of B lymphocytes to a plasma-cell fate is associated with Blimp-1 expression in vivo. J. Immunol. 165, 5462–5471 (2000).
Falini, B. et al. A monoclonal antibody (MUM1p) detects expression of the MUM1/IRF4 protein in a subset of germinal-center B cells, plasma cells and activated T cells. Blood 95, 2084–2092 (2000).
Levens, D. Disentangling the MYC web. Proc. Natl Acad. Sci. USA 99, 5757–5759 (2002).
Martinez-Valdez, H. et al. Human germinal-center B cells express the apoptosis-inducing genes Fas, c-Myc, P53 and Bax, but not the survival gene Bcl-2. J. Exp. Med. 183, 971–977 (1996).
Cutrona, G. et al. The propensity to apoptosis of centrocytes and centroblasts correlates with elevated levels of intracellular myc protein. Eur. J. Immunol. 27, 234–238 (1997).
Dalla-Favera, R., Martinotti, S., Gallo, R. C., Erikson, J. & Croce, C. M. Translocation and rearrangements of the c-myc oncogene locus in human undifferentiated B-cell lymphomas. Science 219, 963–967 (1983).
Akasaka, T. et al. Molecular and clinical features of non-Burkitt's, diffuse large-cell lymphoma of B-cell type associated with the c-MYC/immunoglobulin heavy-chain fusion gene. J. Clin. Oncol. 18, 510–518 (2000).
Hoang, A. T. et al. A link between increased transforming activity of lymphoma-derived MYC mutant alleles, their defective regulation by p107 and altered phosphorylation of the c-Myc transactivation domain. Mol. Cell. Biol. 15, 4031–4042 (1995).
Liu, Y. J. et al. Germinal-center cells express bcl-2 protein after activation by signals which prevent their entry into apoptosis. Eur. J. Immunol. 21, 1905–1910 (1991).
Pezzella, F. et al. Expression of the bcl-2 oncogene protein is not specific for the 14;18 chromosomal translocation. Am. J. Pathol. 137, 225–232 (1990).
Craxton, A., Chuang, P. I., Shu, G., Harlan, J. M. & Clark, E. A. The CD40-inducible Bcl-2 family member A1 protects B cells from antigen receptor-mediated apoptosis. Cell. Immunol. 200, 56–62 (2000).
Karin, M. & Lin, A. NF-κB at the crossroads of life and death. Nature Immunol. 3, 221–227 (2002).
Hinz, M. et al. Constitutive NF-κB maintains high expression of a characteristic gene network, including CD40, CD86 and a set of antiapoptotic genes in Hodgkin/Reed-Sternberg cells. Blood 97, 2798–2807 (2001).
Pahl, H. L. Activators and target genes of Rel/NF-κB transcription factors. Oncogene 18, 6853–6866 (1999).
Tuscano, J. M. et al. Bcl-X rather than Bcl-2 mediates CD40-dependent centrocyte survival in the germinal center. Blood 88, 1359–1364 (1996).
Bakhshi, A. et al. Cloning the chromosomal breakpoint of t(14;18) human lymphomas: clustering around JH on chromosome 14 and near a transcriptional unit on 18. Cell 41, 899–906 (1985).
Tsujimoto, Y., Cossman, J., Jaffe, E. & Croce, C. M. Involvement of the bcl-2 gene in human follicular lymphoma. Science 228, 1440–1443 (1985).
Monni, O. et al. BCL2 overexpression associated with chromosomal amplification in diffuse large B-cell lymphoma. Blood 90, 1168–1174 (1997).
Neri, A. et al. Molecular analysis of cutaneous B- and T-cell lymphomas. Blood 86, 3160–3172 (1995).
Cabannes, E., Khan, G., Aillet, F., Jarrett, R. F. & Hay, R. T. Mutations in the IkBa gene in Hodgkin's disease suggest a tumour suppressor role for IκBα. Oncogene 18, 3063–3070 (1999).
Jungnickel, B. et al. Clonal deleterious mutations in the IκBα gene in the malignant cells in Hodgkin's lymphoma. J. Exp. Med. 191, 395–402 (2000).
Akagi, T. et al. A novel gene, MALT1 at 18q21, is involved in t(11;18) (q21;q21) found in low-grade B-cell lymphoma of mucosa-associated lymphoid tissue. Oncogene 18, 5785–5794 (1999).
Lucas, P. C. et al. Bcl10 and MALT1, independent targets of chromosomal translocation in MALT lymphoma, cooperate in a novel NF-κB signaling pathway. J. Biol. Chem. 276, 19012–19019 (2001).
Uren, A. G. et al. Identification of paracaspases and metacaspases: two ancient families of caspase-like proteins, one of which plays a key role in MALT lymphoma. Mol. Cell. 6, 961–967 (2000).
Zhang, Q. et al. Inactivating mutations and overexpression of BCL10, a caspase recruitment domain-containing gene, in MALT lymphoma with t(1;14)(p22;q32). Nature Genet. 22, 63–68 (1999).
Ruland, J. et al. Bcl10 is a positive regulator of antigen receptor-induced activation of NF-κB and neural-tube closure. Cell 104, 33–42 (2001).
Sylla, B. S. et al. Epstein–Barr virus-transforming protein latent infection membrane protein 1 activates transcription factor NF-κB through a pathway that includes the NF-κB-inducing kinase and the IκB kinases IKKα and IKKβ. Proc. Natl Acad. Sci. USA 95, 10106–10111 (1998).
Krappmann, D. et al. Molecular mechanisms of constitutive NF-κB/Rel activation in Hodgkin/Reed-Sternberg cells. Oncogene 18, 943–953 (1999).
Staudt, L. M., Dent, A. L., Shaffer, A. L. & Yu, X. Regulation of lymphocyte cell-fate decisions and lymphomagenesis by BCL-6. Int. Rev. Immunol. 18, 381–403 (1999).
Dalla-Favera, R. et al. Molecular pathogenesis of B-cell malignancy: the role of BCL-6. Curr. Top. Microbiol. Immunol. 246, 257–263 (1999).
Allman, D. et al. BCL-6 expression during B-cell activation. Blood 87, 5257–5268 (1996).
Cattoretti, G. et al. Bcl-6 protein is expressed in germinal-center B cells. Blood 86, 45–53 (1995).
Dent, A. L., Shaffer, A. L., Yu, X., Allman, D. & Staudt, L. M. Control of inflammation, cytokine expression and germinal-center formation by BCL-6. Science 276, 589–592 (1997).
Ye, B. H. et al. The BCL-6 proto-oncogene controls germinal-centre formation and TH2-type inflammation. Nature Genet. 16, 161–170 (1997).
Fukuda, T. et al. Disruption of the Bcl6 gene results in an impaired germinal-center formation. J. Exp. Med. 186, 439–448 (1997). References 64–66 use Bcl-6-deficient mice to show that Bcl-6 is required for GC formation and that it regulates inflammation.
Shaffer, A. L. et al. BCL-6 represses genes that function in lymphocyte differentiation, inflammation and cell-cycle control. Immunity 13, 199–212 (2000).
Reljic, R., Wagner, S. D., Peakman, L. J. & Fearon, D. T. Suppression of signal transducer and activator of transcription 3-dependent B-lymphocyte terminal differentiation by BCL-6. J. Exp. Med. 192, 1841–1848 (2000).
Vasanwala, F. H., Kusam, S., Toney, L. M. & Dent, A. L. Repression of AP-1 function: a mechanism for the regulation of Blimp-1 expression and B-lymphocyte differentiation by the B-cell lymphoma-6 protooncogene. J. Immunol. 169, 1922–1929 (2002). References 67–69 identify genes that are inhibited by BCL-6 in B cells, including genes that control the cell cycle ( p27KIP1 ) and differentiation ( BLIMP1).
Turner, C. A. Jr, Mack, D. H. & Davis, M. M. Blimp-1, a novel zinc-finger-containing protein that can drive the maturation of B lymphocytes into immunoglobulin-secreting cells. Cell 77, 297–306 (1994).
Shaffer, A. L. et al. Blimp-1 orchestrates plasma-cell differentiation by extinguishing the mature B-cell gene-expression program. Immunity 17, 51–62 (2002). This study shows that BLIMP1 acts as the master regulator of plasma-cell differentiation by extinguishing gene-expression programmes that direct proliferation and GC B-cell functions, such as class-switch recombination. BLIMP1 mediates these broad effects by regulating the expression of other transcription factors directly and by reciprocally repressing BCL6.
Lin, Y., Wong, K. & Calame, K. Repression of c-myc transcription by Blimp-1, an inducer of terminal B-cell differentiation. Science 276, 596–599 (1997).
Niu, H., Ye, B. H. & Dalla-Favera, R. Antigen-receptor signaling induces MAP kinase-mediated phosphorylation and degradation of the BCL-6 transcription factor. Genes Dev. 12, 1953–1961 (1998).
Shvarts, A. et al. A senescence rescue screen identifies BCL6 as an inhibitor of anti-proliferative p19(ARF)–p53 signaling. Genes Dev. 16, 681–686 (2002).
Alexander, K. & Hinds, P. W. Requirement for p27(KIP1) in retinoblastoma protein-mediated senescence. Mol. Cell. Biol. 21, 3616–3631 (2001).
Iida, S. et al. The t(9;14)(p13;q32) chromosomal translocation associated with lymphoplasmacytoid lymphoma involves the PAX-5 gene. Blood 88, 4110–4117 (1996).
Urbanek, P., Wang, Z. Q., Fetka, I., Wagner, E. F. & Busslinger, M. Complete block of early B-cell differentiation and altered patterning of the posterior midbrain in mice lacking Pax5/BSAP. Cell 79, 901–912 (1994).
Nutt, S. L., Heavey, B., Rolink, A. G. & Busslinger, M. Commitment to the B-lymphoid lineage depends on the transcription factor Pax5. Nature 401, 556–562 (1999).
Mikkola, I., Heavey, B., Horcher, M. & Busslinger, M. Reversion of B-cell commitment upon loss of Pax5 expression. Science 297, 110–113 (2002).
Horcher, M., Souabni, A. & Busslinger, M. Pax5/BSAP maintains the identity of B cells in late B lymphopoiesis. Immunity 14, 779–790 (2001). References 77–80 delineate the essential role of PAX5 in committing cells to and maintaining them in the B-cell lineage.
Reimold, A. M. et al. Transcription factor B-cell lineage-specific activator protein regulates the gene for human X-box binding protein 1. J. Exp. Med. 183, 393–401 (1996).
Reimold, A. M. et al. Plasma-cell differentiation requires the transcription factor XBP-1. Nature 412, 300–307 (2001).
Lin, K. I., Angelin-Duclos, C., Kuo, T. C. & Calame, K. Blimp-1-dependent repression of Pax-5 is required for differentiation of B cells to immunoglobulin-M-secreting plasma cells. Mol. Cell. Biol. 22, 4771–4780 (2002).
Vaandrager, J. W. et al. DNA fiber fluorescence in situ hybridization analysis of immunoglobulin class switching in B-cell neoplasia: aberrant CH gene rearrangements in follicle center-cell lymphoma. Blood 92, 2871–2878 (1998).
Lam, K. P., Kuhn, R. & Rajewsky, K. In vivo ablation of surface immunoglobulin on mature B cells by inducible gene targeting results in rapid cell death. Cell 90, 1073–1083 (1997).
Cavalli, F., Isaacson, P. G., Gascoyne, R. D. & Zucca, E. MALT lymphomas. Hematology (Am. Soc. Hematol. Educ. Program) 241–258 (2001).
Wotherspoon, A. C. et al. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet 342, 575–577 (1993).
Bayerdorffer, E. et al. Regression of primary gastric lymphoma of mucosa-associated lymphoid tissue type after cure of Helicobacter pylori infection. MALT Lymphoma Study Group. Lancet 345, 1591–1594 (1995).
Morgner, A. et al. Complete remission of primary high-grade B-cell gastric lymphoma after cure of Helicobacter pylori infection. J. Clin. Oncol. 19, 2041–2048 (2001).
Hussell, T., Isaacson, P. G., Crabtree, J. E. & Spencer, J. The response of cells from low-grade B-cell gastric lymphomas of mucosa-associated lymphoid tissue to Helicobacter pylori. Lancet 342, 571–574 (1993).
Qin, Y. et al. Somatic hypermutation in low-grade mucosa-associated lymphoid tissue-type B-cell lymphoma. Blood 86, 3528–3534 (1995).
Du, M. et al. Ongoing mutation in MALT lymphoma immunoglobulin gene suggests that antigen stimulation plays a role in the clonal expansion. Leukemia 10, 1190–1197 (1996).
Zuckerman, E. et al. Hepatitis C virus infection in patients with B-cell non-Hodgkin lymphoma. Ann. Intern. Med. 127, 423–428 (1997).
Rabkin, C. S. et al. Prospective study of hepatitis C viral infection as a risk factor for subsequent B-cell neoplasia. Blood 99, 4240–4242 (2002).
Hermine, O. et al. Regression of splenic lymphoma with villous lymphocytes after treatment of hepatitis C virus infection. N. Engl. J. Med. 347, 89–94 (2002).
Quinn, E. R. et al. The B-cell receptor of a hepatitis C virus (HCV)-associated non-Hodgkin lymphoma binds the viral E2 envelope protein, implicating HCV in lymphomagenesis. Blood 98, 3745–3749 (2001).
Jaffe, E. S., Harris, N. L., Stein, H., Vardiman, J. W. Tumours of Haematopoietic and Lymphoid Tissues (IARC, Lyon, 2001).
Klein, U. et al. Gene-expression profiling of B-cell chronic lymphocytic leukemia reveals a homogeneous phenotype related to memory B cells. J. Exp. Med. 194, 1625–1638 (2001).
Rosenwald, A. et al. Relation of gene expression phenotype to immunoglobulin mutation genotype in B-cell chronic lymphocytic leukemia. J. Exp. Med. 194, 1639–1648 (2001). References 98 and 99 use gene-expression profiling to show that chronic lymphocytic leukaemia (CLL) is a single disease with at least two variants.
Damle, R. N. et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood 94, 1840–1847 (1999).
Fais, F. et al. Chronic lymphocytic leukemia B cells express restricted sets of mutated and unmutated antigen receptors. J. Clin. Invest. 102, 1515–1525 (1998).
Hamblin, T. J., Davis, Z., Gardiner, A., Oscier, D. G. & Stevenson, F. K. Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood 94, 1848–1854 (1999). References 100–102 define two forms of CLL on the basis of the mutational status of immunoglobulin sequences in the leukaemic cells.
Oscier, D. G., Thompsett, A., Zhu, D. & Stevenson, F. K. Differential rates of somatic hypermutation in V(H) genes among subsets of chronic lymphocytic leukemia defined by chromosomal abnormalities. Blood 89, 4153–4160 (1997).
Rawstron, A. C. et al. Monoclonal B lymphocytes with the characteristics of 'indolent' chronic lymphocytic leukemia are present in 3.5% of adults with normal blood counts. Blood 100, 635–639 (2002).
Tobin, G. et al. Somatically mutated Ig V(H)3-21 genes characterize a new subset of chronic lymphocytic leukemia. Blood 99, 2262–2264 (2002).
Sthoeger, Z. M. et al. Production of autoantibodies by CD5-expressing B lymphocytes from patients with chronic lymphocytic leukemia. J. Exp. Med. 169, 255–268 (1989).
Borche, L., Lim, A., Binet, J. L. & Dighiero, G. Evidence that chronic lymphocytic leukemia B lymphocytes are frequently committed to production of natural autoantibodies. Blood 76, 562–569 (1990).
Kipps, T. J. et al. Developmentally restricted immunoglobulin heavy-chain variable region gene expressed at high frequency in chronic lymphocytic leukemia. Proc. Natl Acad. Sci. USA 86, 5913–5917 (1989).
He, X., Goronzy, J. J., Zhong, W., Xie, C. & Weyand, C. M. VH3-21 B cells escape from a state of tolerance in rheumatoid arthritis and secrete rheumatoid factor. Mol. Med. 1, 768–780 (1995).
Caligaris-Cappio, F. B-chronic lymphocytic leukemia: a malignancy of anti-self B cells. Blood 87, 2615–2620 (1996).
Goodnow, C. C. et al. Self-tolerance checkpoints in B-lymphocyte development. Adv. Immunol. 59, 279–368 (1995).
Bell, S. E. & Goodnow, C. C. A selective defect in IgM antigen-receptor synthesis and transport causes loss of cell-surface IgM expression on tolerant B lymphocytes. EMBO J. 13, 816–826 (1994).
Payelle-Brogard, B., Magnac, C., Alcover, A., Roux, P. & Dighiero, G. Defective assembly of the B-cell receptor chains accounts for its low expression in B-chronic lymphocytic leukaemia. Br. J. Haematol. 118, 976–985 (2002).
Michel, F. et al. Defective calcium response in B-chronic lymphocytic leukemia cells. Alteration of early protein tyrosine phosphorylation and of the mechanism responsible for cell calcium influx. J. Immunol. 150, 3624–3633 (1993).
Zupo, S. et al. CD38 expression distinguishes two groups of B-cell chronic lymphocytic leukemias with different responses to anti-IgM antibodies and propensity to apoptosis. Blood 88, 1365–1374 (1996).
Lankester, A. C. et al. Antigen-receptor nonresponsiveness in chronic lymphocytic leukemia B cells. Blood 86, 1090–1097 (1995).
Healy, J. I. et al. Different nuclear signals are activated by the B-cell receptor during positive versus negative signaling. Immunity 6, 419–428 (1997).
Vilen, B. J., Burke, K. M., Sleater, M. & Cambier, J. C. Transmodulation of BCR signaling by transduction-incompetent antigen receptors: implications for impaired signaling in anergic B cells. J. Immunol. 168, 4344–4351 (2002).
Schuh, K., Avots, A., Tony, H. P., Serfling, E. & Kneitz, C. Nuclear NF-ATp is a hallmark of unstimulated B cells from B-CLL patients. Leuk. Lymphoma 23, 583–592 (1996).
Krober, A. et al. V(H) mutation status, CD38 expression level, genomic aberrations and survival in chronic lymphocytic leukemia. Blood 100, 1410–1416 (2002).
Adams, J. Preclinical and clinical evaluation of proteasome inhibitor PS-341 for the treatment of cancer. Curr. Opin. Chem. Biol. 6, 493–500 (2002).
Letai, A. et al. Distinct BH3 domains either sensitize or activate mitochondrial apoptosis, serving as prototype cancer therapeutics. Cancer Cell 2, 183 (2002).
Mellemkjaer, L. et al. Rheumatoid arthritis and cancer risk. Eur. J. Cancer 32A, 1753–1757 (1996).
Coiffier, B. Diffuse large-cell lymphoma. Curr. Opin. Oncol. 13, 325–334 (2001).
Huang, J. Z. et al. The t(14;18) defines a unique subset of diffuse large B-cell lymphoma with a germinal center B-cell gene-expression profile. Blood 99, 2285–2290 (2002).
Baldwin, A. S. Control of oncogenesis and cancer-therapy resistance by the transcription factor NF-κB. J. Clin. Invest. 107, 241–246 (2001).
Shipp, M. A. et al. Diffuse large B-cell lymphoma outcome prediction by gene-expression profiling and supervised machine learning. Nature Med. 8, 68–74 (2002).
Hagman, J. et al. Pax-5/BSAP: regulator of specific gene expression and differentiation in B lymphocytes. Curr. Top. Microbiol. Immunol. 245, 169–194 (2000).
Usui, T. et al. Overexpression of B-cell-specific activator protein (BSAP/Pax-5) in a late B cell is sufficient to suppress differentiation to an Ighigh producer cell with plasma-cell phenotype. J. Immunol. 158, 3197–3204 (1997).
Rosenwald, A. & Staudt, L. M. Clinical translation of gene-expression profiling in lymphomas and leukemias. Semin. Oncol. 29, 258–263 (2002).
Thorselius, M. et al. Somatic hypermutation and V(H) gene usage in mantle-cell lymphoma. Eur. J. Haematol. 68, 217–224 (2002).
Algara, P. et al. Analysis of the IgV(H) somatic mutations in splenic marginal-zone lymphoma defines a group of unmutated cases with frequent 7q deletion and adverse clinical course. Blood 99, 1299–1304 (2002).
Thiede, C. et al. Ongoing somatic mutations and clonal expansions after cure of Helicobacter pylori infection in gastric mucosa-associated lymphoid tissue B-cell lymphoma. J. Clin. Oncol. 16, 3822–3831 (1998).
Gurrieri, C. et al. Chronic lymphocytic leukemia B cells can undergo somatic hypermutation and intraclonal immunoglobulin V(H)DJ(H) gene diversification. J. Exp. Med. 196, 629–639 (2002).
Acknowledgements
We wish to thank the members of the Staudt lab and the Lymphoma/Leukemia Molecular Profiling Project for discussions and support.
Author information
Authors and Affiliations
Corresponding author
Related links
Related links
DATABASES
Cancer.gov
Entrez
LocusLink
Swiss-Prot
FURTHER INFORMATION
Glossary
- V(D)J RECOMBINATION
-
The somatic rearrangement of variable (V), diversity (D) and joining (J) regions of antigen-receptor genes, which leads to the repertoire diversity of both T- and B-cell receptors.
- GERMINAL CENTRE
-
The structure that is formed by the clonal expansion of antigen-activated B-cell blasts that have migrated to the follicles of lymph nodes. The B cells in these structures proliferate and their immunoglobulin genes undergo somatic hypermutation, before the cells leave as plasma cells or memory B cells.
- FOLLICULAR DENDRITIC CELLS (FDCs).
-
Cells with a dendritic morphology that are present in lymph nodes, where they present intact antigens held in immune complexes to B cells.
- PLASMABLAST
-
A dividing B cell that is committed to plasma-cell differentiation.
- CLASS-SWITCH RECOMBINATION
-
DNA rearrangement of the VDJ region from immunoglobulin M to any of the IgG, IgA or IgE constant genes at the heavy-chain locus. Recombination occurs in repetitive sequences of DNA that are located upstream of each constant gene.
- SOMATIC HYPERMUTATION
-
The substitution of 'untemplated' nucleotides or small deletions targeted to a rearranged VDJ or VJ segment, which occurs only in B cells. The mutations are found between the promoter and enhancer of the rearranged gene (including non-coding regions), but they are found at the highest frequency in 'hotspots' (RGYW) that are located in the complementarity-determining regions.
Rights and permissions
About this article
Cite this article
Shaffer, A., Rosenwald, A. & Staudt, L. Lymphoid Malignancies: the dark side of B-cell differentiation. Nat Rev Immunol 2, 920–933 (2002). https://doi.org/10.1038/nri953
Issue Date:
DOI: https://doi.org/10.1038/nri953
This article is cited by
-
Shared genetic architecture between autoimmune disorders and B-cell acute lymphoblastic leukemia: insights from large-scale genome-wide cross-trait analysis
BMC Medicine (2024)
-
MCL1 as a therapeutic vulnerability in Burkitt lymphoma
Leukemia (2023)
-
IL-1R8 expression in DLBCL regulates NK cell recruitment and influences patient prognosis
Functional & Integrative Genomics (2023)
-
Immunomagnetic B cell isolation as a tool to study blood cell subsets and enrich B cell transcripts
BMC Research Notes (2021)
-
Detailed characterization of the transcriptome of single B cells in mantle cell lymphoma suggesting a potential use for SOX4
Scientific Reports (2021)